Educational Philosophy
Turning a talented medical student into a capable, empathetic surgeon requires a well-designed training program as well as a passion for surgical education. The general surgery residency program at Temple has a strong track record of producing surgeons ready to take on the challenges of clinical practice or the rigors of subspecialty training.
Our unique location provides exposure to a wide variety of pathology, patient populations, and of how social determinants of health impact patient care outcomes. The multiple ancillary sites provide exposure to subspecialty care as well as community-based general surgery.
Each of our clinical rotations provide ample patient care and operative exposure in an environment that prioritizes education over service. Our educators balance the needs of autonomy and supervision for the trainees while maintaining high quality patient care.
Through a process of active and ongoing feedback from residents, faculty and other members of the healthcare team, we continually analyze and alter our educational offerings to reflect the needs of our residents. Recent changes include altering our didactic conference to include small group learning and flipped classroom activities, starting an in-hospital in-situ simulation program and growing our ultrasound training. Feedback is critical in the development of the residents. Real-time feedback is provided during and at the conclusion of a case, and written feedback is given after each rotation. The faculty and residents are encouraged to discuss the resident’s overall progress throughout the rotation.
The success of the Temple general surgery residency can be documented by the fellowships and positions obtained by our graduates, our board passage rate and the community leadership roles that our trainees pursue. But more important is way our residents care about each other, our patients, and our community.
Conferences and Didactics

Our Wednesday morning conference schedule begins with Morbidity and Mortality conference where the department meets to discuss challenging cases and complications. Joint M&M conferences are held periodically with other surgical specialties or the Department of Anesthesia to discuss multidisciplinary cases.
Grand Rounds occurs each week during the academic year and covers a variety of both surgical and non-surgical topics. Lecturers come from both within the Temple University System, other academic institutions and non-medical occupations. The Grand Rounds schedule concludes each year with each Chief Resident presenting on a topic of their choice. Notable recent visiting Grand Rounds speakers include:
- William Walters, MD - Managing Director of Operational Medicine for the Department of State
- Don Smolenski - President of the Philadelphia Eagles
- Joel Fish - Sports Psychologist for the Philadelphia 76ers
- Rachel Levine, MD – (former) Secretary of Health for the Commonwealth of Pennsylvania; current Assistant Secretary for Health for the U.S. Department of Health and Human Services
- Michelle Histand - Director of Innovation at Independence Blue Cross
- Thoalf Sundt, MD - Chief of Cardiovascular Surgery at Massachusetts General Hospital
- Robert Montgomery, MD - Director of the NYU Transplant Institute
- Thomas Scalea, MD - Physician in Chief, Shock Trauma Center
- Jo Buyske, MD – President and Chief Executive Officer of the American Board of Surgery
Skills Lab and Simulation Training

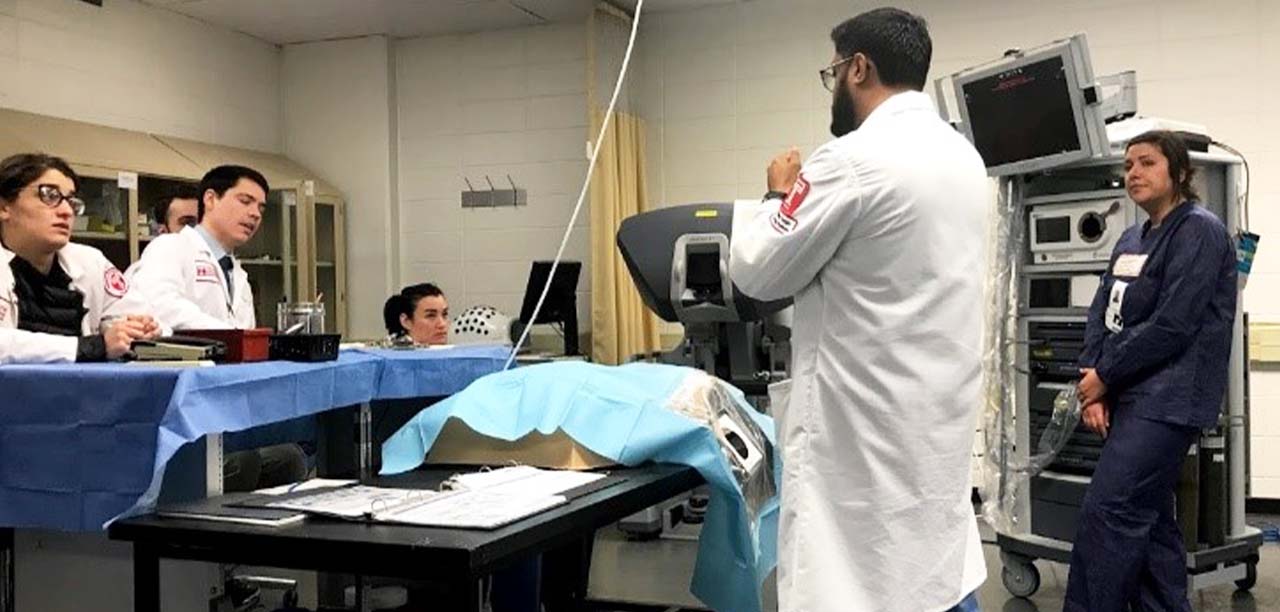
The William Maul Measey Institute for Clinical Simulation and Patient Safety is an American College of Surgeons-accredited Education Institute that provides opportunities for learning both technical and non-technical skills in a simulated environment. Sessions dedicated to technical skills may include central venous catheter insertion, vascular anastomosis, trauma bay skills in an animate model or surgical exposures in a cadaver. Non-technical skill training includes education in informed consent, end of life discussions, stress management and team training. The Simulation Center also serves as a testing center for the Fundamentals of Laparoscopic Surgery and Fundamentals of Endoscopic Surgery exams.
Along with the simulation center, the Robotics Training Center provide educational opportunity in minimally invasive and robotic surgery. This is a dynamic space containing both a DaVinci robotic trainer and an Intuitive robotic simulator, both of which are used in the robotic simulation curriculum.
Our simulation curriculum culminates each year with the Surgical Olympics where resident teams compete in a variety of technical challenges.

Clinical Rotations
The clinical rotations are designed to give each resident a broad-based general surgery experience in the academic and community environments. Each resident will be exposed to general surgical practice and general surgical subspecialties. Through high quality medical care and the use of evidence-based medicine, the residents will learn to provide surgical care using best practices in differing environments and with a diverse patient population.
The third year provides a unique opportunity to complete a clinical elective of the resident’s choice.
Operative Experience

The operative experience provided to Temple surgery residents is one of increasing operative autonomy, often paralleling increases in case and patient complexity. In addition to the core general surgery operations, residents participate in complex vascular and endovascular operations, advanced minimally invasive surgery, robotic general and thoracic cases, complex surgical oncology and endocrine surgery operations, advanced endoscopic procedures, and a high volume of trauma and burn surgery.
Temple surgery residents graduate with case numbers in excess of the minimum requirements of the American Board of Surgery and the ACGME
