Elevating Quality and Safety: An Innovative and Immersive Curriculum
Over the past two decades, the importance of Quality Improvement (QI) and Patient Safety (PS) in healthcare has grown exponentially. Today, these principles are essential not only to clinical excellence but also to practice management, public accountability, and physician compensation. Recognizing this, the ACGME has made QI and PS core competencies for residency training.
At Temple University Hospital, we have developed a robust, integrated QI/PS curriculum that empowers residents to become leaders in clinical improvement and patient-centered care. Our approach is dynamic and mission-driven, shaped by the shared goals of stakeholders across the Temple University Health System:
- Graduate Medical Education (GME) committed to cultivating lifelong learners in QI/PS
- Hospital administration focused on delivering cost-effective, high-quality care
- Faculty dedicated to advancing their own scholarly work and mentorship
- A collective commitment to improving patient outcomes and safety every day
Curriculum Goals and Objectives
- Promote a culture of continuous improvement by making quality and safety a routine part of patient care at Temple University Hospital
- Enhance scholarly engagement by supporting QI/PS projects that are presented at local, regional, or national meetings, and/or submitted for publication
- Prepare residents for independent practice by equipping them with the skills to navigate quality reporting, risk management, and value-based care contracting
Our curriculum ensures that residents leave prepared not only to practice medicine but to improve it. Through hands-on learning, interdisciplinary collaboration, and faculty mentorship, Temple residents develop the tools to drive meaningful change in any healthcare setting.
Framework
Quality Improvement in Action: From Insight to Impact
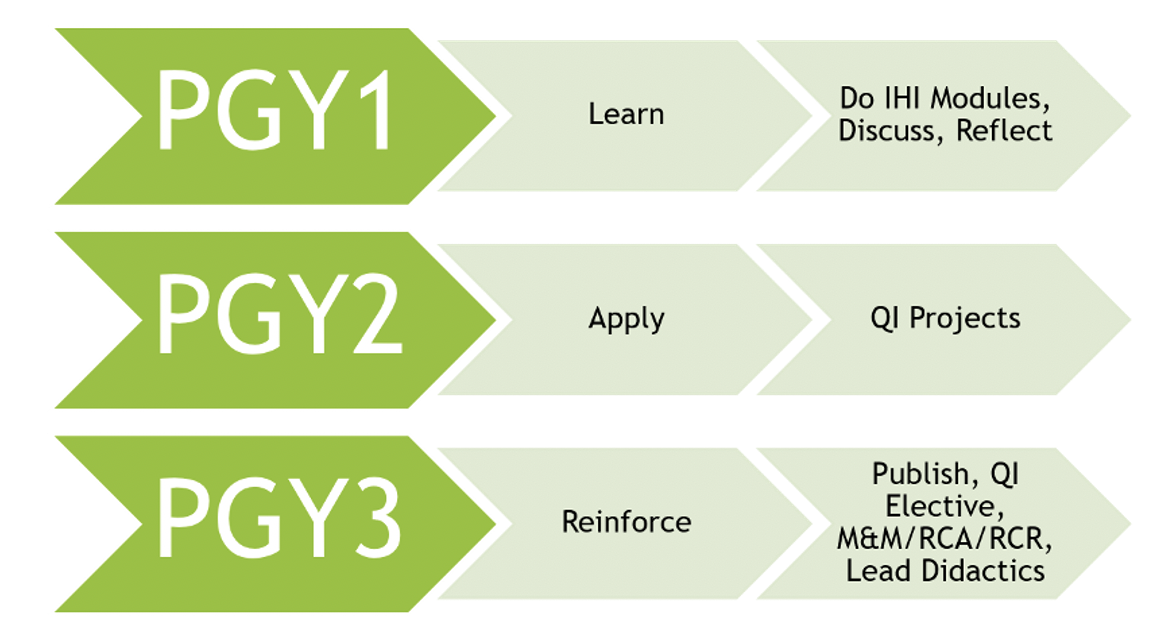
Our QI curriculum is more than a theoretical framework—it's an active, collaborative, and longitudinal experience designed to spark innovation and real-world change. Through a structured series of experiential learning events, residents at all levels contribute to a culture of continuous improvement:
Integrated QI Learning Structure
- Pain-a-thon: Residents across all training levels identify "pain points"—daily challenges or inefficiencies encountered in patient care. These issues are categorized within hospital-aligned domains, setting the stage for meaningful QI projects.
- Hack-a-thon: Rising PGY-2 residents select a pain point of interest and begin conceptualizing their QI project, engaging in problem-solving and systems-based thinking with guidance from faculty mentors.
- Shark Tank: Early PGY-2s formally pitch their QI project proposals to a panel of hospital and health system leaders. This exercise fosters system-level engagement, secures institutional buy-in, and builds early momentum for change.
- Fish Bowl: At the end of the academic year, residents present their QI project outcomes during a capstone event. These presentations showcase results, highlight lessons learned, and promote peer-to-peer learning.
Quality Improvement Scholarship
Our QI projects are not only vehicles for institutional impact but also platforms for professional development. Residents are encouraged and supported in submitting their work to local, regional, and national conferences—building a strong foundation for fellowship or job applications.
Recent venues for resident QI scholarship include:
- Temple’s Sol Sherry Research Symposium
- Society of Hospital Medicine (SHM)
- American College of Physicians (ACP)
- High Value Practice Academic Alliance (HVPAA)
- American College of Cardiology (ACC)
...and many more.
Patient Safety Curriculum: Building a Culture of Safety
Our Goal
To cultivate skilled, safety-conscious physicians who lead with vigilance, transparency, and a commitment to error prevention and continuous improvement.
Curriculum Highlights
- Foundational Education
Core patient safety principles are taught through structured modules adapted from the American College of Physicians (ACP) curriculum. - Systems Integration
Content is brought to life by hospital-based experts who contextualize safety topics using real-world hospital metrics, performance data, and active initiatives. - Applied Learning
Residents lead and participate in:- Root Cause Analyses (RCAs)
- Morbidity & Mortality (M&M) Conferences
- Patient Safety Event Reviews
These forums provide hands-on experience in analyzing adverse events, improving systems, and developing communication strategies that prioritize safe and effective care.
QI/PS Curriculum Leadership:
- Dharmini Shah Pandya, MD (Director of QI/PS curriculum)
- Brianna Graham, MD (Chief Resident for Health Systems Sciences)

