One overdose story in a hospital with far too many
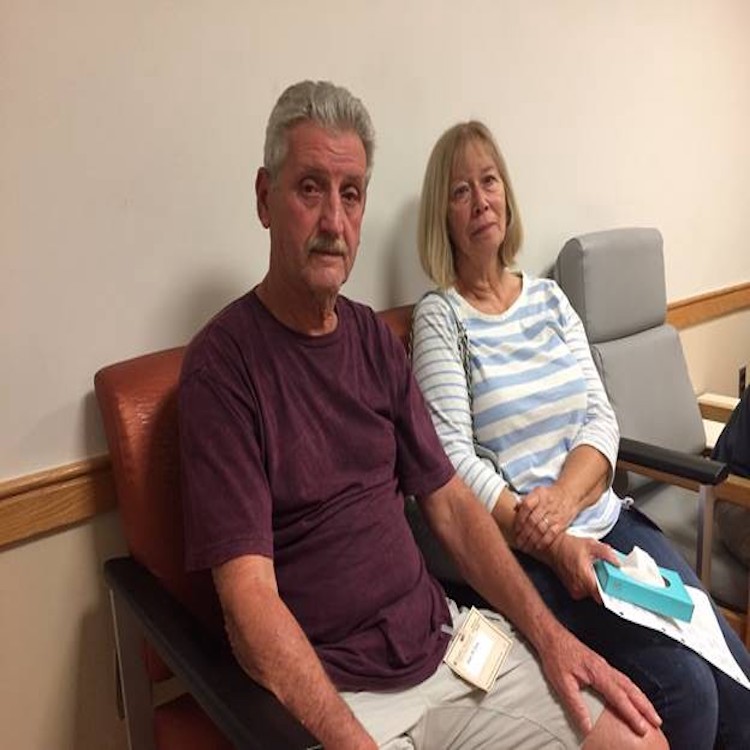
The parents, Neil and Terry McGroarty. Photo by Michael Vitez.
By Michael Vitez
Just after 9 p.m. on a rainy Friday, the announcement came over the public address.
“Attention Episcopal emergency department. Medic 45 in route with a code blue. Male, 35, no vitals. ETA 5 minutes.”
It was like the floor had been tipped and everyone and everything — doctors, nurses, technicians, medicines, machines, even Nina Trimboli, the unit clerk, out of breath, who had just run to find new pads for the defibrillator — flowed to the one room set up for resuscitations at the Episcopal Campus of Temple University Hospital.
Three people lined up to take turns doing chest compressions. Dr. Derek Isenberg opened an app on his iPhone to a metronome, matching the beat of the recently stopped heart.
Paramedics put the stretcher on the bed. The patient’s jeans were so soggy the medical student had trouble cutting them. His beard was trimmed. His feet were bare.
“Start compressions please,” Dr. Isenberg said.
A paramedic gave a report. “Four Epis so far,” he said, referring to doses of epinephrine, used to chemically restart a heart. “Pupils fixed and dilated. Needles found at the scene.”
“Tell me how long he’s been down now?” Dr Isenberg asked.
“About 25 minutes,” said the paramedic.
The man was found on the sidewalk on East Clementine Street. No identification.
Felix Fernandes, the CT and X-ray tech, didn’t recognize him.
Often they’ve overdosed before.
***
As many as 80 overdoses a week get treated at Episcopal, located in the heart of Philadelphia’s Kensington section. The Drug Enforcement Agency calls the area the “biggest open air drug market on the East Coast.”
“Episcopal is absolutely ground zero of all ground zeroes,” said the city’s health commissioner, Dr. Thomas Farley, at a meeting about the opioid crisis with Temple physicians last month.
Doctors at Episcopal estimate that for every overdose patient, another 11 are treated for medical problems in which drug abuse is the root cause — from damaged heart valves to skin infections to pneumonia. Not long ago, an addict came in with maggots in the pressure sores on his rear end. http://bit.ly/2i9QWva He was homeless, living in his wheelchair.
Increasingly, paramedics or police give patients Narcan, a drug that reverses the effect of heroin. The addicts often wake up in the emergency room furious that their highs have been ruined. One doctor texted me, “I get F You 1000x more than thank you.”
“We see so many young people die at Episcopal mainly from drugs and at Temple from trauma,” said Dr. Naomi Rosenberg, an ED attending working at Episcopal on this rainy Friday night. “I don’t have a good answer for how we cope with that. Anything I would say would sound so trite. How any of us deal with human suffering is hard to summarize.”
“The way you deal with it in the moment,” she said, “is to rely on your training.”
***
“Naomi, is the tube good?” asked Dr. Isenberg.
Paramedics had put a breathing tube down the man’s throat and into his lungs.
“We’re checking right now,” responded Dr. Rosenberg.
With the first chest compressions, what Dr. Rosenberg identified as “frothy pulmonary secretions” rose up through that breathing tube and spilled onto the sleeve of Scott Sees, a medical student who started a rotation in the ED that afternoon, and was doing compressions for the first time. Sees ignored his bloody wet sleeve and just kept pushing.
The student had gone to the simulation center earlier in the afternoon to practice on a robot patient for just this moment, and felt incredibly well prepared, but was surprised by how physically hard it was, especially on his core muscles.
“Let’s hold compressions for a rhythm check,” said Dr. Isenberg.
The monitor indicated some heart rhythm. The doctor put the ultrasound over the heart. It showed a heartbeat, but too faint to sustain life.
Nurses rolled the patient on his side, so Dr. Isenberg could check the patient’s back. He thought he saw pooling blood, a sign of death. But the heart did have motion.
As a person dies, cells in the lungs stop producing carbon dioxide.
This man’s C02 readings were normal.
“Keep going with compressions,” Dr. Isenberg said.
He ordered more epinephrine and other drugs.
Eight people in the room worked individually and in concert, hanging medicines, checking monitors, putting in lines, cutting off clothes, keeping a written record of every action. In a way they were as methodical as the metronome.
Then calmly, Dr. Isenberg announced, “he’s got a nice strong pulse now.”
In eight minutes, they had restarted his heart.
“Back to life,” said Felix, the x-ray tech.
Not exactly.
There was no celebration, no joy.
Everyone in the ED knew this man’s brain had gone too long without oxygen.
Yet they continued to work on him, to do everything they could for him. Dr. Rosenberg put in a new, sterile central line so the new resident in the ICU in the middle of the night wouldn’t have to do it. The med student put in a nasogastric tube.
They prepared the patient for transport to the Intensive Care Unit at Temple University Hospital, where neurologists would evaluate his brain status.
“I felt that we gave him a chance,” said Dr. Isenberg.
The medical student was impressed by such calm under pressure. He was so proud to be part of the team. And hopeful. He wondered, “Where does his life go from here?”
***
On Monday, the patient was in room 203 in Temple’s RICU, respiratory intensive care unit. They had done the first exam that morning, and there was no neurological function. He was brain dead. The law requires two exams. A second doctor would do an exam later that day.
Other patients had their names on the white board in the nurse’s station. He had only a number, “5310 M.”
He lay in the hospital bed, under the covers, in a hospital gown, attached to a ventilator. The TV was on “Harry” on Fox 29, and a band was blasting away.
“We keep it on,” said Orion Garcia, the RICU nurse, speaking of the television. “Mostly for us I guess. But you never know.”
Garcia estimated at least two overdose patients a week end up in the ICU. About half get better, she said. And half do not.
She could tell from experience he was a heroin addict. “Drug addicts all get a sickly, tired look,” she said. “I’m sure he was a nice guy. So many of the drug addicts are nice people. It’s too bad.”
That afternoon, Garcia looked over her patient’s body carefully for any identifying tattoos. She found a name, in old English letters, scripted across his shoulder blades. She had a hunch that was his name. She went on Facebook and kept looking at people with that last name until she saw his face.
His Facebook profile listed the last place he worked, sheet metal workers local 19 in Philadelphia. Garcia shared this information with a hospital social worker, who called the union, and urged someone to contact the family and have them call the hospital.
By 6 pm, a man was in room 203. He was older, gray, slight. He had both arms on the bed rail, tears raining down his cheeks. He’d just arrived, just been told. He was the father.
***
Prescriptions for narcotics nearly tripled in Philadelphia from 2001 to 2015, paralleling the increase in overdose deaths, according to Farley, the health commissioner. There is no chance of reducing overdose deaths unless you reduce opioid prescriptions, he said, and suggests doctors cut them by 75 percent.
“We’re trying to get fewer people addicted to pills in the first place,” Farley told Temple doctors in September.
The city is also encouraging hospitals to focus more on use of medication-assisted treatments — such as Suboxone, a daily pill that suppresses both the craving for heroin and the onset of withdrawal now.
“We know these are effective, ” said Rose Julius, the deputy chief medical officer with Community Behavioral Health. “They’re grossly underused.”
A Temple Health task force, convened last winter, presented Farley with its report, “Addressing the Opioid Epidemic.” Temple’s approach is multi-disciplinary, involving research, education, community intervention, and increased services.
One plan is literally to walk overdose victims from the emergency room right into treatment centers on hospital grounds or in the community, and start them on Suboxone in the ED.
There have been some immediate steps. Temple this summer doubled the number of people it treats with Suboxone in its outpatient clinic, and will make it available in the ED and inpatient settings this fall.
Overdose patients also now leave the hospital now with a Narcan spray, so they can revive another addict — or somebody can revive them.
Temple Health also is planning a new approach in addiction medicine, with doctors developing an expertise, like an oncologist or cardiologist — a recognition that addiction is a disease, not a crime.
***
Michael Vitez, winner of the 1997 Pulitzer Prize for Explanatory Journalism at The Philadelphia Inquirer, is the director of narrative medicine at the Lewis Katz School of Medicine at Temple University. Michael.vitez@temple.edu
