Temple-Led Research Team Finds Sex-Based Differences in Utilization and Outcomes for Catheter-Directed Thrombolysis in Patients with Deep Vein Thrombosis
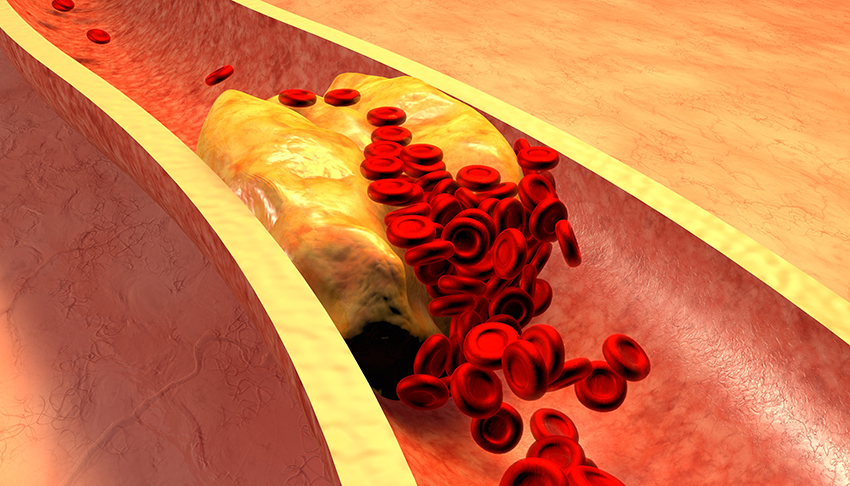
Deep vein thrombosis (DVT) is a serious condition that occurs when a blood clot forms in a vein, often in the deep veins of the legs, thigh or pelvis. Those clots can break loose, travel to the lungs and block blood flow, causing a pulmonary embolism.
The majority of patients with DVT develop it in their lower extremities and that leads to a painful condition known as post-thrombotic syndrome in approximately half of all patients. Post-thrombotic syndrome is marked by pain, swelling, redness and chronic sores in the affected legs. Patients can also develop DVT in a vein carrying deoxygenated blood to the heart from the lower body or from the head, arms and upper body. This is called caval DVT.
One way to treat DVT is a procedure called catheter-directed thrombolysis (CDT), which allows physicians to place a clot-dissolving agent directly into the clot. CDT has become more commonly used in the United States since research showed it reduced the incidence of post-thrombotic syndrome.
Given this increased utilization, a research team led by Riyaz Bashir, MD, FACC, RVT, Professor of Medicine at the Lewis Katz School of Medicine at Temple University and Director of Vascular and Endovascular Medicine at Temple University Hospital, sought to identify and describe sex-based differences in utilization and safety outcomes of CDT for treatment of DVT in the U.S. In research published online by the journal Vascular Medicine, the team found sex-based differences in both utilization and safety outcomes.
“The data provided some interesting findings,” says Dr. Bashir. “In addition to differences in utilization, we were able to find variations in the incidence of a number of complications, including bleeding that requires blood transfusion, intracranial hemorrhage, gastrointestinal bleeding and acute kidney injury, as well as the incidence of angioplasty, stenting, and adjunctive IVC filter placement.”
The research team used the Nationwide Inpatient Sample database to identify 108,243 patients age 18 years or older with a primary discharge diagnosis of proximal lower extremity or caval DVT between January 2005 and December 2011. Of those patients, 4,826 (4.5%) were treated with CDT.
Among the team’s findings:
- Female patients were less likely to be treated with CDT for DVT.
- Female patients experienced more bleeding complications requiring blood transfusion.
- Intracranial hemorrhage, gastrointestinal bleeding and acute kidney injury were more common in male patients.
- Mortality rates were similar for both men and women treated with CDT.
- Women treated with CDT were more likely to undergo angioplasty, stenting and adjunctive IVC filter placement.
“Future research should focus on uncovering why these sex-based differences exist,” says Dr. Bashir. “The answers to those questions could help shape future treatment guidelines for patients who are suitable candidates for CDT.”
