Clinical Rotations
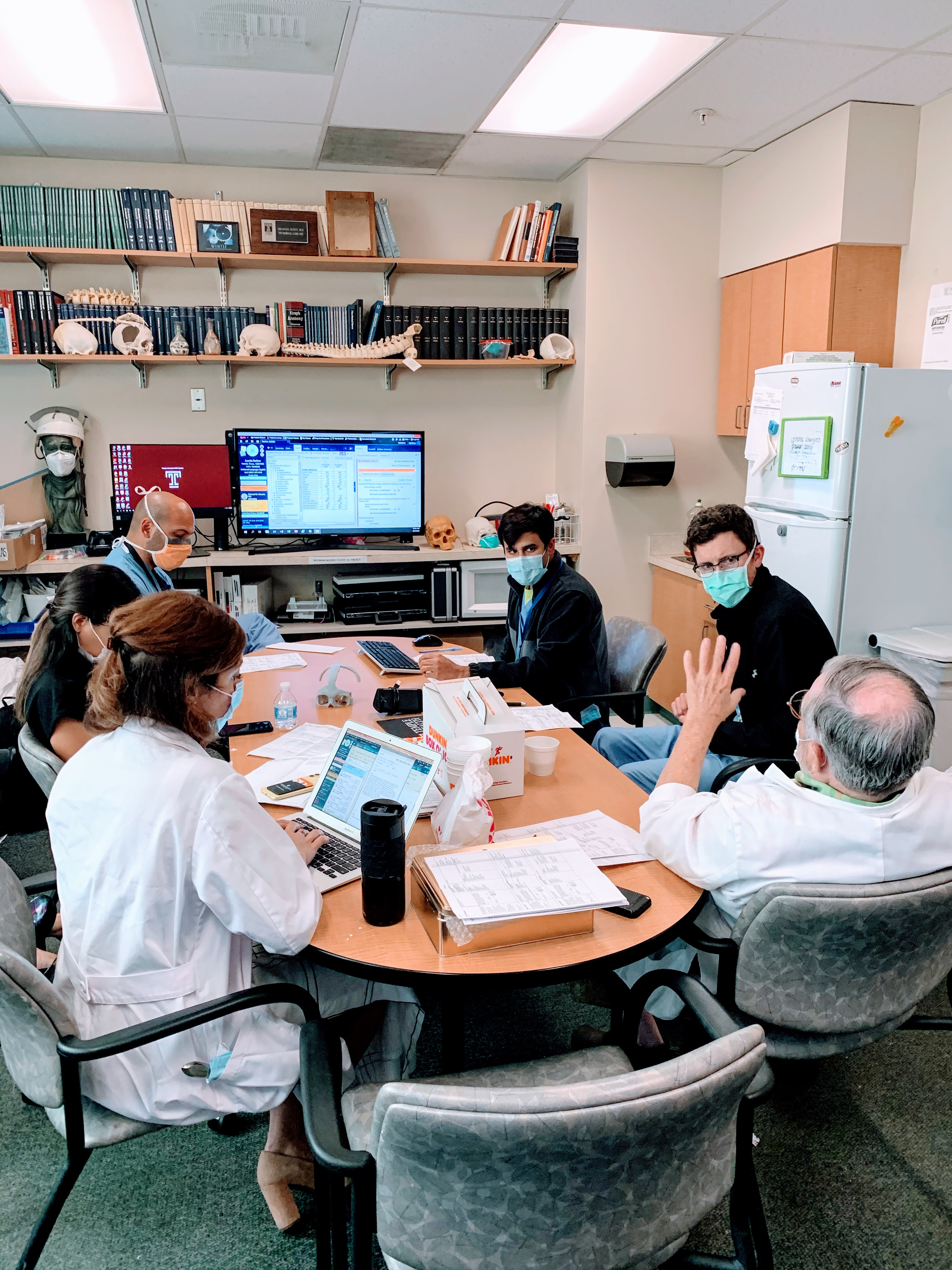 Residents on the Temple Neurosurgery service are expected to progress through the various clinical rotations specified below. These rotations allow the resident to develop the skills and knowledge base required for the well-trained neurosurgeon.
Residents on the Temple Neurosurgery service are expected to progress through the various clinical rotations specified below. These rotations allow the resident to develop the skills and knowledge base required for the well-trained neurosurgeon.
Residents work primarily at Temple University Hospital, TUH – Jeanes Campus, and Fox Chase Cancer Center. Temple residents also spend 6 months during their PGY-4 year at the Children’s Hospital of Philadelphia (CHOP).
Rotations
PGY-1
- Neurology: 3 months
- ENT/Neuroradiology/Neuropathology: 3 months
- Neuro ICU: 6 months
The neurosurgery intern spends the first part of the year rotating with our colleagues in neurology, ENT, neuroradiology, and neuropathology. They then begin their dedicated time in the neurosurgery service taking on the role of the neuro-trauma & neuro-critical care resident. During this time, they are the primary resident involved with managing patients in the Neurosurgery ICU and continue to do so for a total of 12 months. The intern plays an essential role in the service caring for our sickest patients, seeing and staffing common general neurosurgery consults, and performing bedside procedures such as external ventricular drains (EVDs), central venous lines, arterial lines, shunt programming and tapping, lumbar punctures and lumbar drains. Becoming proficient in these skills is paramount as they begin to take ‘buddy calls’ with senior residents during their off-service time prior to taking solo-in house calls beginning in January of the intern year. Our interns are motivated to become efficient at managing tasks to get into the operating room for assisting in simple neurosurgery cases.
PGY-2
- Neuro ICU: 6 months
- Cerebrovascular/Endovascular: 6 months
The PGY-2 resident is a seasoned veteran in managing the neurosurgery service, neuro-critical care, and all common bedside procedures. During this year residents spend more time in the operating room becoming proficient at simple cranial and spine surgeries as able and are encouraged to scrub cases with senior residents for more complex cases. Working with senior residents is an invaluable learning experience to grasp technical and operative nuances difficult to glean from textbooks. The second half of the PGY-2 year is spent on the cerebrovascular service both in the angiography suite as well as the operating room. The cerebrovascular resident learns how to perform simple diagnostic angiograms and participate in complex endovascular and open cerebrovascular interventions. The resident will spend time in the cerebrovascular clinic and begin to gain an understanding of how to appropriately manage cerebrovascular lesions in an outpatient context and an opportunity for longitudinal multi-dimensional patient care both pre and post-operatively. Additionally, the CV resident helps to run our bi-weekly CV conference presented in grand rounds style to both neurology and neurosurgery residents. PGY-2 residents are involved with approximately 150-200 cases per year.
PGY-3
- Neuro-Oncology: 6 months
- Spine/Functional: 6 months
The PGY-3 resident is a role model for their junior residents and spends 6 months of the year on the neuro-oncology followed by 6 months on the spine/ functional service. During this time, residents have the opportunity to learn how to manage complex cranial and spinal tumor patients and are involved with the basic functional procedures. The neuro-oncology resident helps to run our weekly neuro-oncology tumor conference, a multidisciplinary conference held along with neurology, neuroradiology, radiation, and medical oncology. They begin to participate more regularly in complex craniotomies and generally become much more technically proficient and confident with these procedures. It is not uncommon for PGY-3 residents to perform between 200-300 cases.
PGY-4
- Cerebrovascular/Endovascular: 6 months
- Pediatric Neurosurgery (CHOP): 6 months
The PGY-4 resident returns to the CV service and is expected to quickly progress from where they last left. It is not uncommon for residents to participate in vascular/endovascular cases during their time on other services however even if limited they quickly become re-acquainted with independently performing simple diagnostic angiograms and build their endovascular skill set to become involved with more complex cases and both simple and complex interventions. They get experience with assisting and performing middle meningeal artery embolization, endovascular treatment of cerebral and spinal vascular malformations, stroke thrombectomy, management of carotid disease with carotid stent and endarterectomy as well as the full gamut of open surgical management of cerebrovascular disease. In January of the PGY-4 year, the resident goes to the Children’s Hospital of Philadelphia for 6 months of pediatrics training. This world-renowned institution provides world-class training. Residents rotate with colleagues from the University of Pennsylvania and Thomas Jefferson University neurosurgery programs. During their time they become well versed in the operative management of hydrocephalus, craniofacial deformities, Moya Moya disease, AVMs, vein of Galen malformations, brain tumors, epilepsy, and movement disorders, tethered cord, myelomeningoceles, spinal deformity, Chiari malformations, and trauma. The PGY-4 resident is expected to perform in a more independent fashion and typically performs ~300 cases during this time.
PGY-5
- Spine/Functional: 6 months
- Neuro-Oncology: 6 months
The PGY -5 resident is the senior resident on service and provides a great opportunity to be a mentor to the junior residents. The 5th year resident does take up to 5 in-house calls per month. They spend the year becoming technically proficient in both anterior and posterior approaches to the spine as well as become more accustomed to MIS posterior and lateral approaches. In addition, they take a much more independent role in surgery for the more complex cranial oncological procedures and spinal instrumentation anywhere from the occiput to the sacrum. The obligations of the spine and neuro-oncology resident may remain the same however their function on service becomes more progressively independent on their way to becoming a chief residents. PGY-5 residents will perform about ~300 cases per year.
PGY-6
- Chief Resident, TUHS Neurosurgery service: 12 months
The neurosurgery chief resident is responsible for the day-to-day operation of the neurosurgery service. They are responsible for the care of every patient on service. The chief sets the tone and culture for how the service functions and its role in the hospital. They spend this year becoming independent with medical and surgical decision-making as well as junior resident teaching both in formal and informal settings. They help make operative case assignments for junior residents and preside over morning reports and evening sign-out with junior residents for the floor/ICU and consult patients
During this year they spend time mastering all simple cranial and spine cases and becoming proficient and independent with complex cranial, spinal, and vascular surgeries to better prepare them for their next step either in post-graduate fellowship or becoming an attending neurosurgeon. Chief residents typically will be involved with the most complex cases performed during the day and typically will be scrubbed with a junior resident for these cases to provide an opportunity for peer mentoring and teaching for the simpler portions of cases. Chief residents typically perform between 300-400 cases.
PGY-7
Research Track: 12 months
Residents are welcome to pursue bench and or clinical research projects throughout residency however this time provides them a more structured longitudinal opportunity to dive into the research process with a minimal clinical obligation. They will still participate in chief calls from time to time however time is utilized to focus on writing articles, applying for funding, and participating in national conferences. Recently, research has been done in collaboration with labs at our home institution as well as Jefferson, Penn, and CHOP.
Or
- Enfolded Fellowship Track: 12 months
Residents have the opportunity to pursue enfolded fellowships within the PGY7 year in neurosurgical sub-specialties including Neuro-endovascular surgery, Spine Surgery, neuro-oncology, or Critical Care/Trauma. The enfolded fellowships are designed to allow residents to obtain certificates of subspecialty training during the 7-year residency program.
