Research Programs
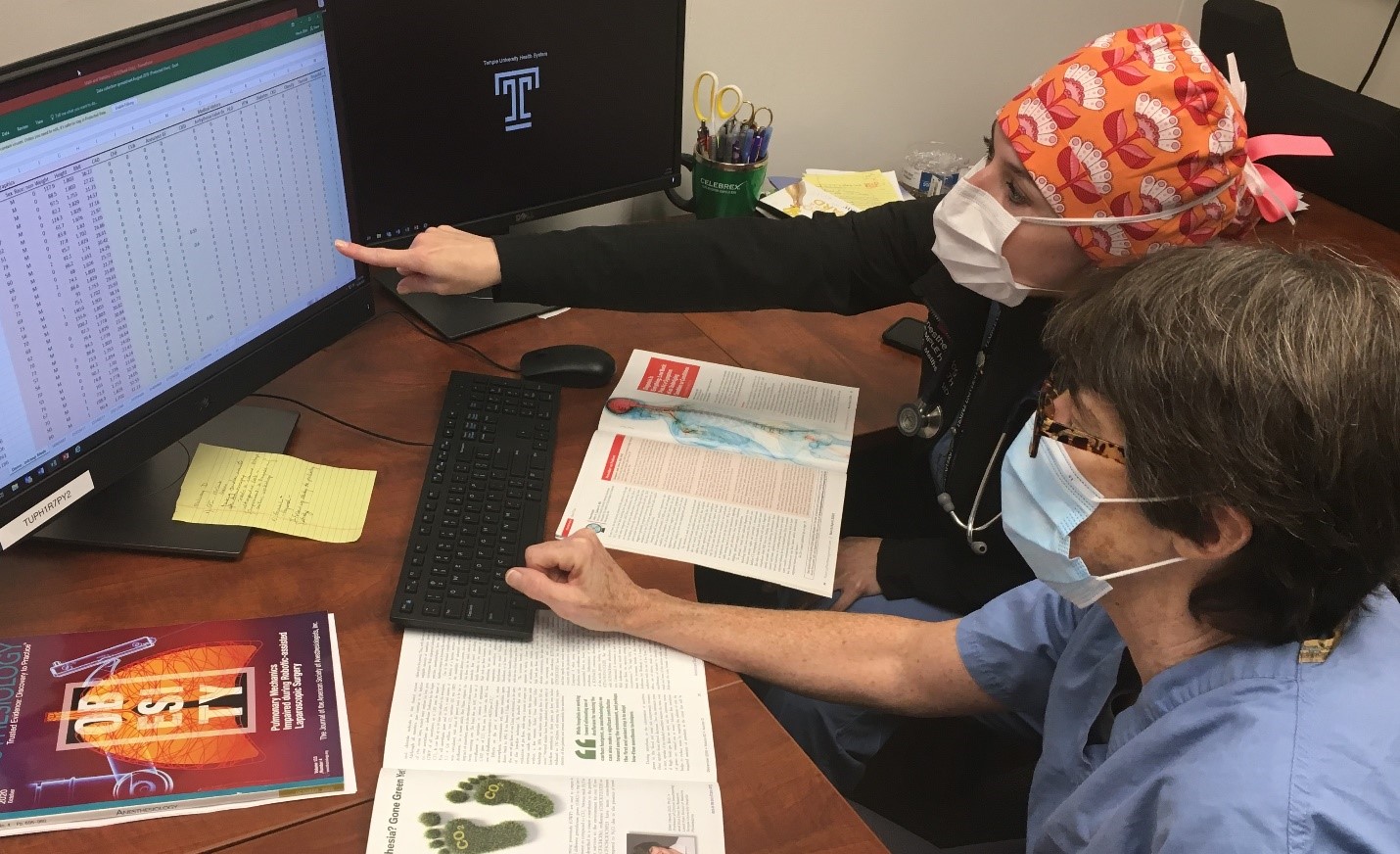 Current research efforts in our department encompass clinical and translational research, and opportunities exist for interested residents and faculty to work on basic research projects in collaboration with faculty at the Lewis Katz School of Medicine. It is an expectation that all residents will become familiar with the essential aspects of clinical study design and execution during the course of their training. Monthly research meetings are mandatory for all residents and participation in ongoing projects or initiation of new protocols is encouraged.
Current research efforts in our department encompass clinical and translational research, and opportunities exist for interested residents and faculty to work on basic research projects in collaboration with faculty at the Lewis Katz School of Medicine. It is an expectation that all residents will become familiar with the essential aspects of clinical study design and execution during the course of their training. Monthly research meetings are mandatory for all residents and participation in ongoing projects or initiation of new protocols is encouraged.
The department of Anesthesiology fosters collaborative efforts with scientists from other departments within the medical school including the Center for Inflammation, Translational and Clinical Lung Research, The Center for Substance Abuse Research, the Department of Plastic Surgery and the Department of Obstetrics and Gynecology.
Research Training
Our department is committed to educating our medical students and residents in the methods of clinical research to enhance their understanding of the medical specialty and encourage contributions to the future improvement of patient care through research.
Medical Students
Each summer we host 2-4 summer interns who have just completed their first year of medical school. These students work are mentored by our faculty, each working on an individual project as well as assisting on several other projects as interest and time allows. Throughout the summer these students learn the process of research protocol design, writing an IRB, informed consent as well as data collection and analysis. Students also get a look at clinical anesthesiology through shadowing in our ORs, pain clinics and ICUs.
Residents
Opportunities for resident driven research are numerous as the research interests of our faculty expand. All our residents participate in research, whether assisting in an ongoing project or initiating their own study.
Basic Research
Pursuing an interest in basic research related to the field of anesthesiology through collaborations with faculty at the Lewis Katz School of Medicine is encouraged. Planning for such a pursuit would begin in the first year of residency.
Industry Sponsored Clinical Research
Through the Temple Clinical Research Institute (TCRI), all the services necessary for faculty to engage in industry sponsored clinical research are available. In addition, our department offers full time research coordinator support. We currently have several faculty members involved in such trials either as a principle investigator or a co-investigator.
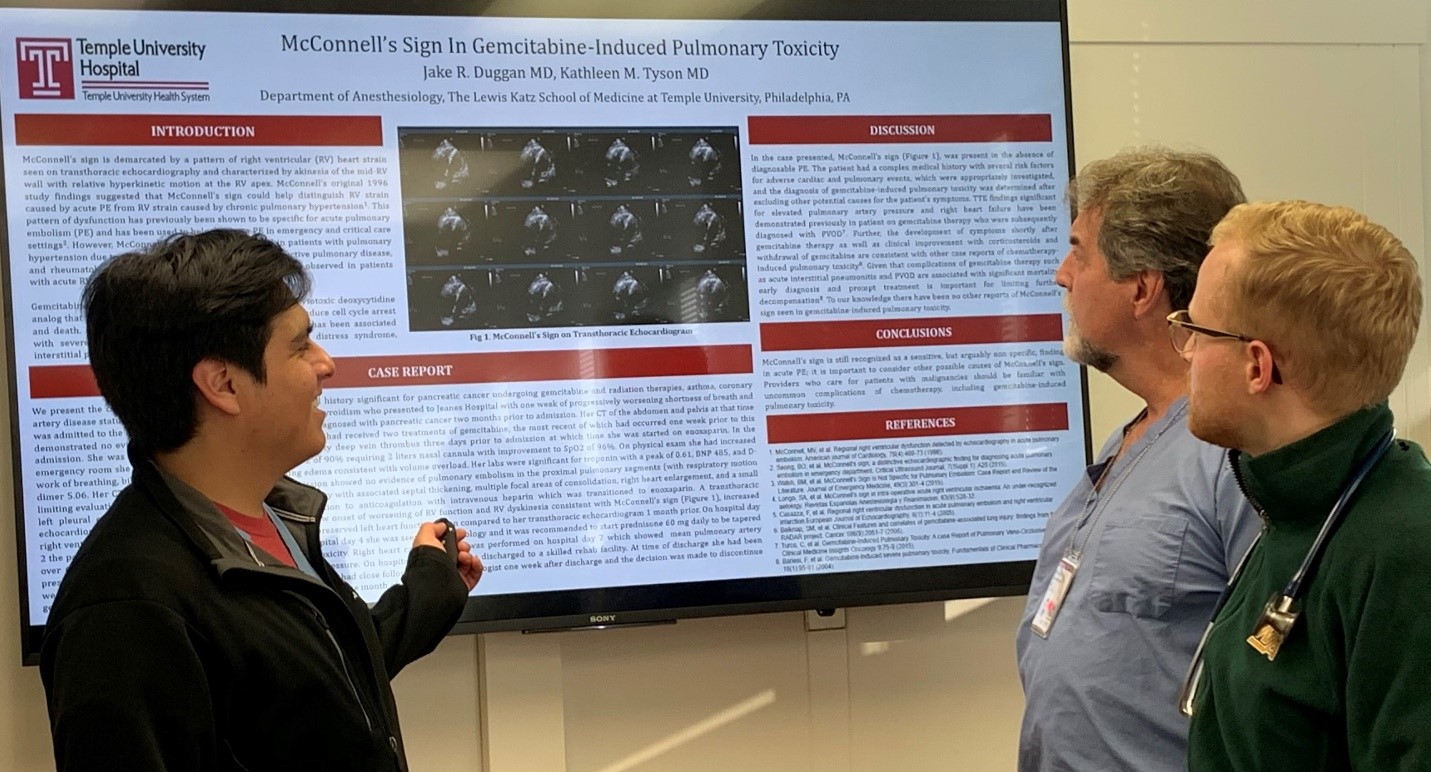
Clinical and Translational Research
A core focus of our research practice is grounded in clinical and translational research. It is a development forum that is relatable to both the provider, the patient and the health care system. This work is fundamental to the physician’s connection to improved patient care.
Some of our current faculty and their areas of research interest include:
Dr. Yuliana Salamanca- Padilla
Investigational focus: Lung transplantation – allocation policies, patient outcomes.
Dr. Kamardeen Alao
Investigational focus: COVID-19 – treatment protocols.
Dr. Gordon Morewood
Investigational focus: ERAS protocols; neuromuscular blockers – cardiac surgery.
Dr. David Fish
Investigational focus: Sepsis –patient outcomes.
Dr. Anish Sethi
Investigational focus: Peripheral nerve blockade and opioid usage.
Dr. Jon Livelsberger
Investigational focus: Peripheral nerve blockade – post-operative care; THC/CBD.
Dr. Ihab Kamel
Investigational focus: Psychological impact of COVID-19; failed spinal anesthesia.
Dr. Abiona Berkeley
Investigational focus: Law, ethics and medicine; Curriculum development – investigational, problem-centered.
Dr. Eric Wilkens
Investigational focus: Medical crisis management – triage protocols; resource management.
Dr. Valerie Armstead
Investigational focus: Healthcare diversity and inclusion; THC/CBD; Wellness.
Dr. Ellen Hauck
Investigational focus: Geriatric medicine – medications impacting the central nervous system; societal and cultural determinants.

